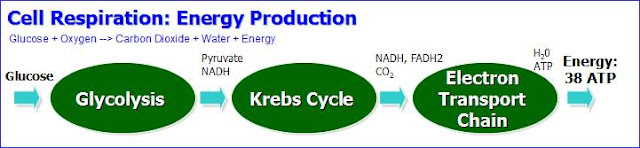
In order to produce
energy, your cells carry out cell respiration within the mitochondria,
which are the power generators of a cell, converting oxygen and
nutrients (glucose, amino acids and fats) into chemical energy
known as adenosine triphosphate (ATP).
With this process your cells produce 38 molecules of ATP; and, then, your cells use this ATP to perform its daily functions.
Why Cancer Patients Waste Away
At least 50% of all cancer patients suffer from a wasting syndrome called cachexia. Affected patients lose weight, including muscle, no matter how much they eat. The wasting is the immediate cause of about one third of all cancer deaths.
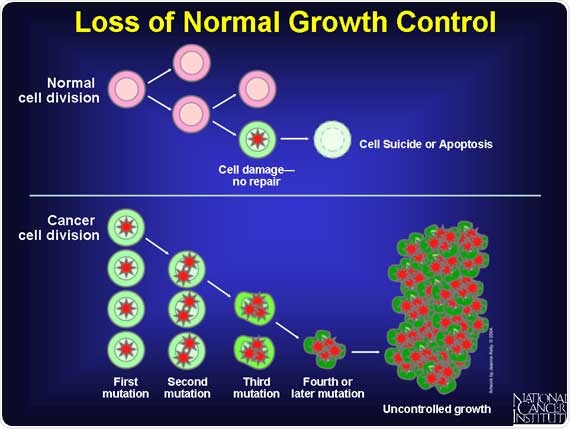
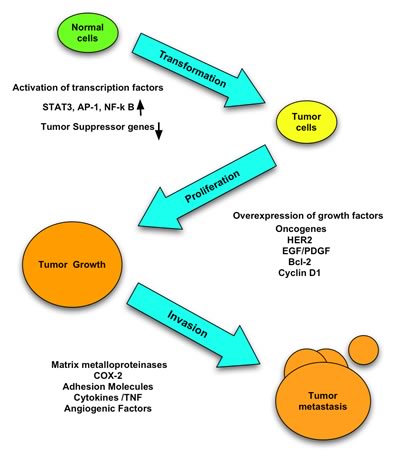
It appears that the cancer cells intervene and consume the majority of the glucose and other nutrients while the normal cells starve. After the cancer cells convert the glucose to energy, the cells secrete lactic acid, which is sent to the liver which converts it back to glucose and returned to the cancer cells, which continue to divide and grow out of control.
In addition, the cancer cells secrete a protein (called IMPL2), which prevents healthy normal cells from responding to insulin, the hormone that stimulates cells to import sugar and burn it for energy. When levels of IMPL2 rise, fat, muscle and other tissues can no longer consume sugar and begin to waste away. Lowering IMPL2 levels reduces the amount of wasting.
Those stark numbers have spurred research into what exactly causes cachexia in patients with cancer and how it might be avoided with a new drug.
The good news is that there are natural substances that can block the production of lactic acid and break the cycle. See below for details.
Cachexia Cycle (Lactic Acid Cycle)
As previously mentioned, the cancer cells (and the microbes inside the cell) interrupt the glucose coming into the cell and consume
(ferment) most of the glucose without oxygen. As part of this
(inefficient) fermentation process, the cancer cells produce less
energy along with lactic acid.
Fermentation allows the cancer cells to produce energy without the need for oxygen. But, the cancer cells are very inefficient at processing glucose -- only about 5% compared to a normal cell. Instead of producing 38 molecules of ATP, each cancer cell (which is now acidic) produces only 2 molecules of ATP, meaning that the cancer cells are wasting a lot of energy.
This wasted energy causes the cancer patient to become tired and malnourished. This excessive use of glucose by a cancer cell is actually part of the process whereby cancer cells actually “steal” glucose from normal cells (cancer cells also steal nutrients from normal cells). This means that normal cells can literally starve to death, creating malnutrition, pain, other health complications and eventually death.
In addition, as a byproduct of the fermentation process, the cancer cells dump lactic acid back into the bloodstream.
Then, the lactic acid is sent to the liver where the liver converts the lactic acid into glucose.
Then, the liver releases the glucose into the bloodstream where cancer cells are likely to pick up this glucose because cancer cells consume about 15 times more glucose than normal cells.
While this may seem like a harmless cycle, there are three reasons why almost half of all cancer patients die from this cycle.
First, the conversion of glucose to lactic acid by the cancer cells and the conversion of lactic acid to glucose in the liver both consume massive amounts of energy.
Second, the lactic acid itself, while it is in the bloodstream, can block key nutrients from reaching healthy (non-cancerous) cells.
Third, the cancer cells secrete a protein (IMPL2), which prevents healthy normal cells from responding to insulin and being able to import sugar and burn it for energy.
To summarize, cachexia is the wasting away of the cancer patient’s body. The cancer metabolizes glucose inefficiently, turning it into lactic acid, which is converted back to glucose by the liver. This process consumes an enormous amount of the body’s energy, causes pain and tires out the cancer patient. This happens over and over again as the cancer grows and the rest of the body wastes away.
Summary
To summarize this process and the cycle:
- The cancer cells ferment massive amounts of glucose, which consumes energy,
- They process the glucose with fermination, which is very inefficient,
- A byproduct of this fermentation is lactic acid,
- This lactic acid then goes into the liver,
- The liver then converts this lactic acid back into glucose, consuming even more energy.
- The cancer cells secrete a protein that prevents normal cells from being able to absorb glucose.
- Much of this glucose is consumed by the cancer cells and the cycle starts over.
Cachexia is seen frequently with cancer, but is also seen with diseases such as AIDS/HIV, heart failure, emphysema, and kidney failure. With regard to cancer, it is seen most frequently with lung cancer, pancreatic cancer, and stomach cancer.
According to the National Cancer Institute, cachexia is estimated to be the immediate cause of death in 20% to 40% of cancer patients, with failure of the respiratory muscles as a frequent cause of death. In addition, about eight out of every ten patients with advanced cancer will suffer from this potentially deadly wasting syndrome.
Cachexia not only worsens survival for people with cancer, but it interferes with quality of life. People with cachexia are less able to tolerate treatments, such as chemotherapy, and often have more side effects. For those who have surgery, postoperative complications are more common. Cachexia also worsens cancer fatigue, one of the most annoying symptoms of cancer.
Cachexia peels away both the visible muscle (somatic muscle) and the invisible muscle (the visceral proteins in the gut and elsewhere). And because the visceral muscle serves as a reservoir for certain immune-enhancing nutrients, the loss of this muscle leads to a weakening of your immune system, making you more prone to life-threatening infections such as pneumonia.
To further complicate matters, many patients suffer from anorexia (a moderate to severe aversion to food) at the same time that they have cachexia. As a result, cancer patients may lose up to 80% of body fat and skeletal muscle. Muscle loss leads to weakness, immobility of patients, more infections and poorer response to treatment. Emotionally, cachexia promotes feelings of fatigue, depression and worthlessness.
A number of factors often converge to cause catabolic wasting. Malnutrition due to reduced food consumption or impaired nutrient absorption occurs frequently in later stages of chronic disease and can cause marked loss of muscle and fat tissue. Even though cachexia is typically accompanied by loss of appetite, it rarely responds to increased food intake alone (Siddiqui 2006; Solheim 2013). Dehydration is another important contributor, as loss of fluid results in reduced weight (Morley 2006).
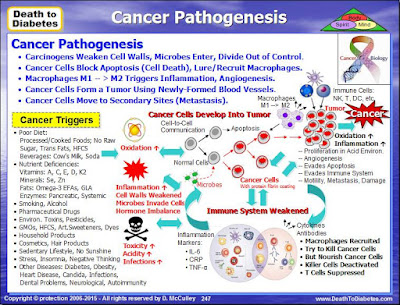
Inflammation also plays a major role in deterioration of body mass among individuals with cachexia (Morley 2006). Both acute and chronic illness can cause marked increases in the production of inflammatory cell-signaling molecules called cytokines. These inflammatory mediators alter numerous metabolic processes, resulting in reduced muscle protein synthesis and increased muscle protein breakdown.
Several specific cytokines have been linked to cachexia including interleukin-1, interleukin-2, interleukin-6, interferon-γ, and tumor necrosis factor-alpha (TNF-α). Inflammatory cytokines activate a major metabolic regulator called nuclear factor kappa B (NF-κB), which in turn drives several physiological changes that promote tissue deterioration.
Inflammatory cytokines also stimulate the release of the adrenal hormone cortisol and neurotransmitter hormones called catecholamines; both cortisol and catecholamines can exacerbate catabolic wasting by disrupting muscle cell metabolism and altering the basal metabolic rate (Siddiqui 2006; Morley 2006).
Reductions in levels of testosterone and insulin-like growth factor-1 (IGF-1) are thought to play an important role in catabolic wasting as well. Both testosterone and IGF-1 exert anabolic actions in muscle tissue, so declining levels of these hormones can lead to reduced muscle mass (Morley 2006).
Note 1: Be careful with glucose-rich intravenous feeding.
This feeds the cancer more than it feeds you. Moreover, overfeeding of
glucose/dextrose can lead to liver and
respiratory problems. A Harvard doctor, George Blackburn, who has
studied nutrition in cancer for several decades, recommends a tailored prescription of macronutrients and micronutrients of 30% lipids, including a minimum of no less than 4-6%
Omega-6 fatty acids and some Omega-3 fatty acids, now known to counter
wasting in cancer. Also, please keep in mind that intravenous feeding, being invasive, offers a route for
blood-borne infections.
Note 2: Before now, cachexia, characterized by muscle wasting and dramatic weight loss, was believed to spare the heart. But an Ohio State University study showed that the condition reduces heart function and changes the heart muscle structure in mice with colon cancer. The study results support the idea that insufficient heart performance might also
be responsible for fatigue symptoms, leading to less exercise and more
severe muscle wasting. The study is published in an issue of the International Journal of Oncology.How to Stop Cachexia
Recommendations from many cancer organizations encourage patients to eat whatever they want of the typical American diet; that is, more saturated fats, refined flours and sugars. But, all that does is feed the inflammation and fuel this muscle-wasting process and make the cachexia even worse!
Stopping or fixing cachexia is not a matter of simply eating more calories, from fats, carbs or protein. Rather, the disorder is a metabolic dysfunction driven by a chronic, low-grade pro-inflammatory condition with the unrelenting and consequent breakdown of muscle and other lean tissues.
Various biofactors have been identified as mediators of tissue wasting in cachexia. As previously mentioned, these include cytokines such as tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), interferon-γ (IFN-γ) and leukemia inhibitory factor (LIF).
Additional factors include tumor-derived factors such as lipid mobilizing factor (LMF) and protein mobilizing factor (PMF), which can directly mobilize fatty acids and amino acids from adipose tissue and skeletal muscle respectively.
It appears that anti-inflammatory supplementation like Omega-3 EFAs (especially eicosapentaenoic acid (EPA)), turmeric/curcumin, ginger, and others, can make a pronounced impact on stopping and reversing this distressful disorder. And, in spite of the fatigue that many patients will experience, gentle resistance exercise is essential to maintain and rebuild fragile muscles.
A sound plant-based nutritional strategy will not only help curtail inflammation, but reduce free-radical damage, minimize platelet activation (which can lead to dangerous blood clotting), manage blood sugar surges, and reduce serum levels of insulin-like growth factor 1 (IGF-1), which stimulates cell multiplication and inhibits cell death.
In addition, some studies have indicated that MSM and Vitamin C were able to reduce lactic acid; and, a substance called hydrazine sulfate was able to break the cachexia cycle. This was accomplished by the hydrazine sulfate being able to block a key enzyme in the liver to prevent lactic acid from getting converted back into glucose.
Athletes and Lactic Acid
Any athlete is familiar with lactic acid. Athletes normally take pickle juice, D-Ribose, MSM (methylsulfonylmethane) and Vitamin C or other special things to get nutrients past the lactic acid blockade and thus get energy into the cells.
Most cancer patients do not die from the cancer cells, rather they die from the damage to the non-cancerous cells. Thus, it is critical to get nutrients past the lactic acid blockage to nourish the non-cancerous cells immediately!!
Every cancer patient who thinks they may have cachexia, no matter what protocol they are on, should start taking D-Ribose immediately. Ribose is an essential ingredient in the formation and conservation of ATP, ADP and AMP (energy molecules).
Note:
ATP = Adenosine triphosphate (3 phosphates attached)
ADP = Adenosine Diphosphate (2 phosphates attached)
AMP = Adenosine monoposphate (1 phosphate attached)
Concerning the buildup of lactic acid, many athletes prior to a strenuous workout, and after the workout, will consume MSM (methylsulfonylmethane) with Vitamin C. This combination is known to neutralize the lactic acid buildup after the workout and it stops the pain.
Using the MSM and Vitamin C together, as they work synergistically, should have the same ability to neutralize the lactic acid in patients with cachexia as well. MSM and vitamin C can be purchased at the health food store. Some MSM products, such as the Trimedica brand, have Vitamin C in the capsule along with the MSM and should work well.
Hydrazine Sulfate
Hydrazine sulphate breaks this lactic acid cycle by blocking a key enzyme in the liver to prevent lactic acid from getting converted back into glucose.
http://www.alkalizeforhealth.net/cancerpain.htm
Note: Of all of the alternative treatments for cachexia, perhaps Hydrazine Sulfate is the best known. The reason is that it was designed specifically for cachexia.
Hydrazine sulfate is the salt of hydrazine and sulfuric acid. Known by the trade name Sehydrin, it is a chemical compound that has been used as an alternative medical treatment for the loss of appetite (anorexia) and weight loss (cachexia) which is often associated with cancer.
Hydrazine sulfate has not been approved in the United States as safe and effective in treating any medical condition, although it is marketed as a dietary supplement. It is also sold over the Internet by websites that promote its use as a cancer therapy. The active ingredient is hydrazine, and the sulfate component is present to aid in formulation.
Hydrazine Sulfate works on stopping the cycle just mentioned. Hydrazine Sulphate, or more commonly Hydrazine Sulfate, interrupts the ability of the liver to convert lactic acid from tumors into glucose thereby helping to starve the tumors and inhibit their ability to metastasize.
Overall gluconeogenesis is stimulated when cancer is present. Gluconeogenesis requires a great deal of energy and excessive gluconeogenesis is thought to be a significant factor that contributes to cancer cachexia (Gold, 1968). Dr. Joseph Gold recognized in the 1960’s that metabolic strategies that inhibited the enzyme phosphoenol pyruvate carboxykinase (PEP-CK) would reduce gluconeogenesis and decrease the severity of cachexia (Gold, 1968). Dr. Gold after testing a series of compounds found that hydrazine sulfate could effectively reduce excessive gluconeogenesis in cancer (Gold, 1974, 1981).
By stopping the liver from converting the lactic acid into glucose breaks the cachexia cycle.
Dr Joseph Gold looked at the chemical process of glycogenesis and determined that, if he inhibited the PEP CK enzyme (much too large a word for anyone to try to pronounce), he could stop the process. Voila, he came up with hydrazine sulfate, a substance that is made cheaply, simple to use, and shrinks tumors. In his early animal studies, Dr Gold showed that, in greater than fifty percent of cancerous animals, he was able to stop the process of glycogenesis, end the cachexia, and the animals began gaining weight. With sugars cut off to the tumor, the tumors began shrinking.
http://www.mnwelldir.org/docs/cancer1/altthrpy2.htm
Warning! Hydrazine Sulfate may raise your blood pressure and heart beat dramatically and cause the worst headache you’ve ever experienced. This is a very dangerous condition, especially for someone already battling cancer.
Hydrazine Sulfate is an MAOI (Momoamine Oxidase Inhibitor). What it does is inhibit an enzyme that breaks down monoamines (serotonin, norepinephrine, and dopamine), those brain chemicals that make us happy. MAO inhibitors have been used as antidepressants. However, MAOs have another job in the body: they metabolize tyramine, an amino acid. When taking an MAO inhibitor, tyramine is not broken down, and eating foods with tyramine can raise your blood pressure and heart beat dramatically and cause the worst headache you’ve ever experienced.
Most of the foods containing tayramine are not on most cancer diet plans, so you should be avoiding them anyway.
Foods containing tyramine are (mainly) aged, fermented, or pickled, such as most cheeses (except cottage cheese, cream cheese, and fresh Mozzarella), lunch meats, hot dogs, yogurt, wines and beers. Here is a pretty good list of foods that contain tyramine:
In general, any high protein
food that has undergone aging should be avoided. Also, any
over-the-counter cold or allergy remedy should also be avoided.
http://www.mnwelldir.org/docs/cancer1/altthrpy2.htm
http://www.mnwelldir.org/docs/cancer1/altthrpy2.htm
Here is the warning from Walter Last:
Hydrazine
sulphate is a monoamine oxidase inhibitor and the following should not
be used during hydrazine therapy: tranquilizers or sedatives in doses
greater than 100 mg per day, especially benzodiazepines and
phenothiazines should be avoided, also antihistamines, alcohol and other
agents that depress the central nervous system such as morphine. Also
vitamin B6 should not be taken. Foods high in tyramine must be avoided.
These are aged and fermented products such as most cheeses, cured meats
or fish, sour cream and yoghurt, tofu and tempeh, bouillon cubes,
sauerkraut, pickles and yeast extracts. Also restricted are broad beans,
avocados, bananas, raisins, figs, dates and dried fruit in general as
well as overripe fruit.
http://users.mrbean.net.au/~wlast/cancer6-remedies.html
Here is the warning of Dr. Gold, developer of Hydrazine Sulphate:
Here is the warning of Dr. Gold, developer of Hydrazine Sulphate:
HS
is an irreversible and potent MAO (monoamine oxidase) inhibitor, a
class of compounds that can have potentially deadly interactions with
other drugs. For over three decades it has been known that central
nervous system depressants—such as barbiturates, tranquilizers and
alcohol—are incompatible with MAO inhibitors and use of the two together
could result in extremely dangerous effects.
Note: For details about using Hydrazine Sulfate, refer to the Hydrazine Sulfate Protocol on the Cancer tutor website:
Cesium Chloride
One option to help hydrazine sulfate stop this lactic acid cycle is alkalinity. Cesium chloride (and a few other minerals), the most common substance to make cancer cells alkaline in an alkaline treatment program, has been proven by Dr. A. Keith Brewer, PhD, to get into cancer cells, when other nutrients cannot. The cesium chloride:
-- Makes the cancer cell alkaline,
-- Limits the intake of glucose into the cell (thus starving the cell),
-- Neutralizes the lactic acid (which is actually what causes the cell to multiply uncontrollably and eventually kills the cell) and makes it nontoxic, and
-- Stops the fermentation process, which is a second affect of limiting the glucose (fermentation is what creates lactic acid in the first place).
In other words, cesium chloride will break the cycle in several different ways.
But this is the important point: Hydrazine Sulfate blocks the cachexia cycle in the liver and cesium chloride blocks the cachexia cycle in the cancer cells.
Both cesium chloride and hydrazine sulfate are complex treatments and have many restrictions.
Refer to the the following website for more details:
http://www.cancertutor.com/hydrazine/
Other Website References About Cachexia
Cachexia (Lactic Acid Cycle)
http://www.canceractive.com/cancer-active-page-link.aspx?n=3429
http://www.clinicalcorrelations.org/?p=1285
http://www.tpims.org/disease-research/wasting-syndrome
http://mobile.the-scientist.com/article/42601/insulin-interference-triggers-cancer-linked-cachexia
http://msccc.com/cancer-resources/nutrition-in-cancer-care
http://www.doctorsacrossborders.mu/diseases/item/613-cancer-and-cachexia-silent-killer-wasting-disease.html