Although there are many forms of cancer, for the most part, most cancers develop in similar ways and use similar methods.
It is now becoming more widely accepted that cancer is
not pre-programmed into your genes, but rather it is the environment of
your body that regulates your genetic expression that can trigger cancer
to occur.
Adverse epigenetic influences that can negatively affect cell division and damage or mutate DNA
and alter genetic expression, allowing cancer to proliferate, include
the following factors:
-- Chronic inflammation
-- Free radical damage (oxidative stress)
-- Hormonal imbalances
-- Toxins and pollution
-- Chronic infections -- Nutritional deficiencies
-- Chronic stress; negative thoughts and emotional conflicts
-- Other health issues, e.g. diabetes, obesity, autoimmune disease
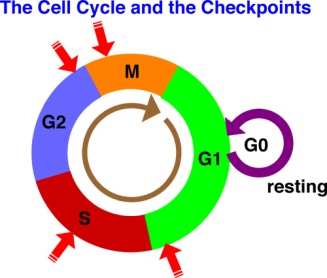
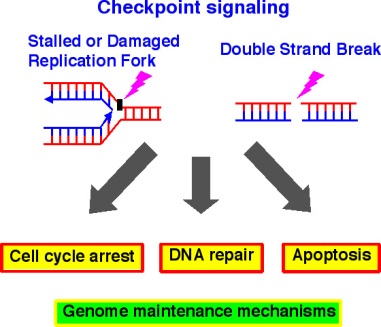
Cell Division
The most common form of cell division is called
mitosis.
It is used for growth and repair. During mitosis, a cell makes an exact
copy of itself and splits into two new cells. Each cell contains an
exact copy of the original cell's chromosomes in their 23 pairs. This is
the reason why all the cells in an organism are genetically identical.
Cells do not live forever -- they follow a normal cell cycle and they will reach a point where they will
divide through mitosis, or die through a process called apoptosis.
There are two types of genes that normally control the cell cycle:
proto-oncogenes,
which start cell division and
tumor-suppressor genes, which turn off cell
division. These two genes work together, one turning on cell division
when the body needs to repair or replace tissue, and the other turning
off cell division when the repairs have been made. If the
proto-oncogenes become mutated, they can become
oncogenes -- genes that
lead to uncontrolled cell division. Mutations in the tumor-suppressor
genes result in the cell not having the ability to turn off cell
division.
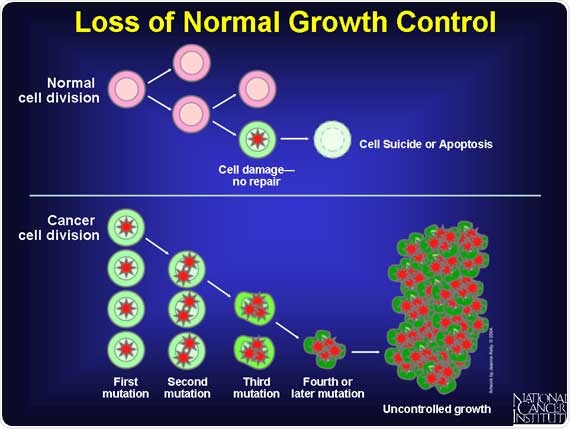
Cancer: Cell Division (Mitosis) Out of Control
Cancer
cells are the exception, these cells do not die and divide
uncontrollably as they crowd out healthy, productive cells. Cancer can
have many causes, but most are thought to be related to carcinogens in
the environment.
Carcinogens are substances that can weaken the immune system and weaken the cell
wall -- allowing the cell wall to become damaged or penetrable from microbes and other
pathogens (e.g. bacteria, viruses, fungi) in the body. (Carcinogens may include
foods, beverages, chemicals, tobacco, environmental toxins, medications,
pesticides, cosmetics, etc.)
Scenario #1: When a
cell becomes weak and is bombarded by free radicals (via inflammation
and/or oxidative stress from carcinogens, toxins, etc.) for years, this
oxidation causes damage to the cell and its nucleus and each time the
cell divides, there is some DNA/gene damage that is not corrected and
repaired and is passed on to the next cell division. This continues
until a mutation occurs that causes the cell to start dividing out of
control and apoptosis (cell death) is blocked. And, if this process
continues over many years, then, the damaged cell may eventually turn
cancerous.
Scenario #2: When a cell becomes weak and is
bombarded by free radicals
(via inflammation and/or oxidative stress from carcinogens, toxins,
etc.) for years, the weakened cell wall may be penetrated by
pathogens/microbes, which cause damage inside the cells, including an
increase in oxidation that causes damage to the
cell and its nucleus and each time the cells divide, there is some
DNA/gene damage that is not corrected and repaired and is passed on to
the next cell division. This continues until a mutation occurs that
causes the cell to start dividing out of control and apoptosis (cell
death) is blocked. And, if this process continues over many years, then,
the damaged cell may eventually turn cancerous.
These
pathogens/microbes are believed to initially be harmless -- until after
years of the body accumulating various toxins and causing
cellular/tissue damage in combination with other events (e.g. high
stress, insomnia, weight gain, inflammation, oxidation, other diseases),
these microbes transform into harmful microbes. It is believed that
these microbes are pleomorphic, that is they have the ability to assume
different forms in response to environmental conditions and changes.
When these microbes are
able to penetrate the cell wall, they interrupt and consume the glucose
going to the mitochondria (the cell's powerhouse) and begin to multiply.
As they multiply, they excrete poisonous mycotoxins creating a very
acidic environment inside the cell. In the meantime, the cell becomes
"tired" because the mitochondria is unable to produce energy (ATP). At
this point, the cell has become cancerous.
When some of the microbes penetrate the cell's nucleus, this causes damage to the cell's DNA/genes and
interferes with the cell's normal cycle, thus disrupting the cell's ability
to control when and how often it divides.
Mitosis is
closely controlled by the genes inside every cell. But, if the DNA/genes
are damaged, this tight control over mitosis is lost and the
newly-formed cancerous cell divides out of control. And, when the
cancerous cell divides, it replicates the damage it just created and
includes some of the microbes in each of the new cancerous cells.
These
cancer cells continue to replicate rapidly without the control systems
that normal cells have plus they don't have the built-in suicide program
(apoptosis) that normal cells have after dividing x number of times.
Instead the cancer cells never trigger apoptosis.
With each
succeeding division, the cancer cells accumulate more genetic mistakes that
make the tumor grow bigger, invade local tissues and eventually spread
(metastasize) to other parts of the body.
The cancer
cells produce less energy (2 ATP molecules vs 38 ATP molecules for a
normal cell) and, as a byproduct of the glucose fermentation, most types
of cancer cells dump lactic acid into the bloodstream. The lactic acid
is sent to the liver, which converts it to glucose and returns the
glucose back to the cells. This cycle can tire out a cancer patient and
cause his body to begin wasting away. Refer to the Lactic Acid Cycle
blog post for more details.
In
addition, the cancer cells release their own enzymes that help the cell
form a slimy, protein covering that "hides" the cancer cells from the
immune system. The immune system contains several types of immune cells
(white blood cells), some of which have the ability to kill foreign
cells, bacteria and other pathogens. For more details, refer to the blog
post about the immune system.
Note: The anatomy
of a cancer cell is different than a normal cell. Morphologically,
the cancer cell is characterized by a large nucleus,
having an irregular size and
shape, the nucleoli are prominent, the cytoplasm is
scarce and intensely colored or pale. For more details, refer to the
blog post Cancer Cell Anatomy.
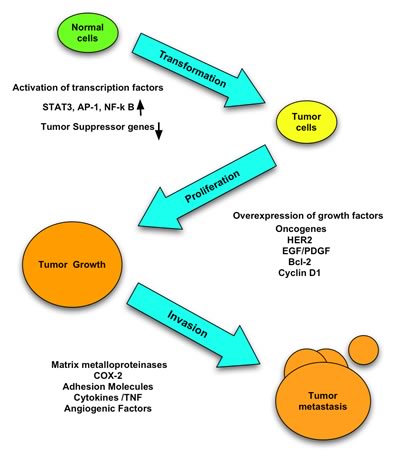
Cancer Tumor Development
Eventually,
the cancer cells form lumps, or tumors, which use the lactic acid to grow and cause damage to the
surrounding tissues. As the tumor gets bigger, the center of it gets
further and further away from the blood vessels in the area where it is
growing. So the center of the tumor gets less and less of the oxygen and
the other nutrients all cells need to survive.
Like
healthy cells, cancer cells cannot live without oxygen and nutrients
although they prefer an anaerobic environment to to grow. In order to
obtain nutrients, the cancer cells send out signals or recruit our own
macrophages (from the immune
system) to trigger an inflammation response and send out signals (called
angiogenic growth factors). These signals encourage new blood vessels
to form and grow into the tumor. This is called angiogenesis. Without a
blood supply, a tumor cannot grow much bigger than a pin head.
Once
a cancer can stimulate blood vessel growth, it can grow bigger and grow
more quickly and produce even more lactic acid. The tumor will stimulate the growth of hundreds of new
capillaries from the nearby blood vessels to bring it nutrients and
oxygen.
Tumor Growing and Spreading
As a
tumor gets bigger, it takes up more room in the body and can then cause
pressure on surrounding structures. It can also grow directly into body
structures nearby. This is called local invasion.
Some
normal cells (e.g. immune cells) produce chemicals called enzymes that
break down cells and tissues. The cells use the enzymes to attack
invading bacteria and viruses. They also use them to break down and
clear up damaged areas in the body. The damaged cells have to be cleared
away so that the body can replace them with new ones. This is all part
of the natural healing process.
Many cancers contain
larger amounts of these enzymes than normal tissues. Some cancers also
contain a lot of normal white blood cells, which produce the enzymes.
The white blood cells* are part of the body's immune response to the
cancer.
One of the things that makes cancer cells
different to normal cells is that they (and the microbes inside) can
move about more easily. This makes it easier for cancer to spread to
another part of the
body to form
multiple secondaries or metastases.
*
Note: There are
several different types of white blood cells that are part of the immune
system. The immune system responds to infection, or anything else the
body
recognizes as 'foreign'. Refer to the blog post that explains how the
immune system and its cells function.
Cancer and Oxygen
Cancer,
above all other diseases, has countless secondary causes. But, even for
cancer, there is only one primary cause. Summarized in a few words, the
prime cause of cancer is the replacement of the respiration of oxygen
in normal body cells by a fermentation of sugar. All normal body cells
meet their energy needs by respiration of oxygen, whereas cancer cells meet their energy needs in great part by fermentation. All normal body cells are thus obligate aerobes, whereas all cancer cells are partial anaerobes."
Poor oxygenation comes
from a buildup of carcinogens and other toxins within and around cells,
which blocks and then damages the cellular oxygen respiration mechanism.
Clumping up of red blood cells slows down the bloodstream, and
restricts flow into capillaries. This also causes poor oxygenation. Even
lack of the proper building blocks for cell walls, Omega 3 essential
fatty acids, restricts oxygen exchange.
Warburg and other
scientists found that the respiratory enzymes in cells, which make
energy aerobically using oxygen, die when cellular oxygen levels drop
to.
When the mitochondrial enzymes
get destroyed, they're host cell can no longer produce all its energy
using oxygen. So, if the cell is to live, it must, to some degree,
ferment sugar to produce energy. For a short period of time, like when
running a race, this anaerobic fermentation of sugar is okay. Your legs
build up lactic acid from this fermentation process and burn, and you
stop running. Then your cells recover and produce energy using oxygen.
However the problem comes when your cells cannot produce energy using
oxygen because of this damage to the respiratory enzymes. Then they must
produce energy primarily by fermentation most of the time. This is what
can cause a cell to turn cancerous.
According to Warburg, cells that produce energy by fermenting sugars may turn cancerous. Warburg's contention is this...
The cells that cannot
produce energy aerobically, cannot produce enough energy to maintain
their ability to function properly. So they lose their ability to do
whatever they need to do in the body.
Fermentation allows
these cells to survive, but they can no longer perform any functions in
the body or communicate effectively with the body. Consequently, these
cells can only multiply and grow. And may become cancerous. Or perhaps
it would be more accurate to say, they degrade into cancer cells that no
longer serve your body, but live to survive...
Decades ago, two
researchers at the National Cancer Institute, Dean Burn and Mark Woods,
(Dean translated some of Warburg's speeches) conducted a series of
experiments where they measured the fermentation rate of cancers that
grew at different speeds. What they found supported Dr. Warburg's
theory.
- See more at: http://www.cancerfightingstrategies.com/oxygen-and-cancer.html#sthash.s35ok650.QfSwbilj.dpuf
The link between oxygen and cancer is clear. In fact, an underlying cause of cancer is
low cellular oxygenation levels.
In
newly formed cells, low levels of oxygen damage respiration enzymes so
that the cells cannot produce energy using oxygen. These cells can then
turn cancerous.
In 1931 Dr. Warburg won his first Nobel
Prize for proving cancer is caused by a lack of oxygen respiration in
cells. He stated in an article titled "The Prime Cause and Prevention of
Cancer...the cause of cancer is no longer a mystery, we know it occurs
whenever any cell is denied 60% of its oxygen requirements..."
"Cancer,
above all other diseases, has countless secondary causes. But, even for
cancer, there is only one primary cause. Summarized in a few words, the
prime cause of cancer is the replacement of the respiration of oxygen
in normal body cells by a fermentation of sugar. All normal body cells
meet their energy needs by respiration of oxygen, whereas cancer cells
meet their energy needs in great part by fermentation. All normal body
cells are thus obligate aerobes, whereas all cancer cells are partial
anaerobes."
Poor oxygenation comes from a buildup of
carcinogens and other toxins within and around cells, which blocks and
then damages the cellular oxygen respiration mechanism.
Clumping up of red blood cells slows
down the bloodstream, and restricts flow into capillaries. This also
causes poor oxygenation. In addition, the proper building blocks for
cell walls, Omega-3 essential fatty acids, restricts oxygen exchange.
When
the mitochondrial enzymes get destroyed, they're host cell can no
longer produce all its energy using oxygen. So, if the cell is to live,
it must, to some degree, ferment sugar to produce energy. For a short
period of time, like when running a race, this anaerobic fermentation of
sugar is okay. Your legs build up lactic acid from this fermentation
process and burn, and you stop running. Then your cells recover and
produce energy using oxygen. However the problem comes when your cells
cannot produce energy using oxygen because of this damage to the
respiratory enzymes. Then they must produce energy primarily by
fermentation most of the time. This is what can cause a cell to turn
cancerous.
The cells that cannot produce energy
aerobically, cannot produce enough energy to maintain their ability to
function properly. So they lose their ability to do whatever they need
to do in the body.
Fermentation allows these cells to
survive, but they can no longer perform any functions in the body or
communicate effectively with the body. Consequently, these cells can
only multiply and grow. And may become cancerous. Or perhaps it would be
more accurate to say, they degrade into cancer cells that no longer
serve your body, but live to survive...
Decades ago,
two researchers at the National Cancer Institute, Dean Burn and Mark
Woods, (Dean translated some of Warburg's speeches) conducted a series
of experiments where they measured the fermentation rate of cancers that
grew at different speeds. What they found supported Dr. Warburg's
theory.
The cancers with the highest growth rates had
the highest fermentation rates. The slower a cancer grew, the less it
used fermentation to produce energy.
Low oxygen levels
in cells may be a fundamental cause of cancer. There are several reasons
cells become poorly oxygenated. An overload of toxins clogging up the
cells, poor quality cell walls that don't allow nutrients into the
cells, the lack of nutrients needed for respiration, poor circulation
and perhaps even low levels of oxygen in the air we breathe.
Cancer
cells produce excess lactic acid as they ferment energy. Lactic acid is
toxic, and tends to prevent the transport of oxygen into neighboring
normal cells. Over time as these cells replicate, the cancer may spread
if not destroyed by the immune system.
Chemotherapy and
radiation are used because cancer cells are weaker than normal cells
and therefore may die first. However, chemo and radiation damage
respiratory enzymes in healthy cells, and overload them with toxins, so
they become more likely to develop into cancer! The underlying cancer
causing conditions are
worsened, not improved. And the cancer usually returns quickly and stronger unless you make changes to support the health of your body.
The
implication of this research is that an effective way to support the
body's fight against cancer would be to get as much oxygen as you can
into healthy cells, and improving their ability to utilize oxygen.
Raising the oxygen levels of normal cells would help prevent them from
becoming cancerous. And increasing oxygen levels in cancer cells to high
levels could help kill those cancer cells.
A nurse who
works in medical research said, "It's so simple. I don't know why I
never thought of it before. When we're working with cell cultures in the
lab, if we want the cells to mutate, we turn down the oxygen. To stop
them, we turn the oxygen back up."
But, it is not easy
to get additional oxygen into cells. Most approaches don't work well.
Breathing oxygen is still limited by the amount of hemoglobin available,
and pH levels. Dr. Whittaker points out, quite rightly, that liquid
oxygen supplements that release oxygen into the blood, which most of
them only do, can't get oxygen into the cells.
He
explains that a delivery mechanism is needed to transport oxygen into
cells. And though the typical oxygen supplement gets oxygen into the
blood, that doesn't mean it gets into the cells.
There
are several ways to significantly increase oxygen levels in your cells
so that you can kill cancer cells and also prevent them from spreading.
The most effective way is to use a hydrogen peroxide protocol (under the
care of a healthcare professional) or take an oxygen supplement that
will literally produce much more oxygen in your cells.
A safer way is to eat sulfur-based foods (e.g. Brussels sprouts, garlic) along with Omega-3 rich foods (e.g. wild
salmon, flax oil, cod liver oil) that will make the cell walls more
permeable. And, eat chlorophyll-rich foods (e.g. wheatgrass, chlorella) along with the Omega-3s to help transport
more oxygen to the cells. And use substances such as MSM, cesium chloride, pancreatic enzymes, etc. to
help penetrate the cell walls of cancer cells.
Note: Refer to the specific treatment protocols that explain this in detail.
You
can also increase the efficiency of the mitochondria, enabling it to
utilize the oxygen to create energy aerobically. The mitochondria that
become damaged by the lack of oxygen cannot produce energy using oxygen,
leading to the development of cancerous cells.
And
finally, you can enhance circulation, reduce blood viscosity and reduce
cellular inflammation so that more oxygen and vital nutrients get to
your cells. By increasing oxygen in your cells, and its utilization, you
will go a long way towards eliminating cancer.
How Cancers Grow and Spread
If left untreated, cancers often go through three stages:
1. Local growth and damage to nearby tissues
Cancer
cells multiply quickly. A cancerous (malignant) tumor is a lump or
growth of tissue made up from cancer cells. Cancerous tumors normally
first develop in one site - the primary tumour.
However, to get larger, a
tumor has to develop a blood supply to obtain oxygen and nourishment
for the new and dividing cells. In fact, a tumor would not grow bigger
than the size of a pinhead if it did not also develop a blood supply.
Cancer cells make chemicals that stimulate tiny blood vessels to grow
around them which branch off from the existing blood vessels. This
ability for cancer cells to stimulate blood vessels to grow is called
angiogenesis.
Cancer cells also have the ability to push through
or between normal cells. So, as they divide and multiply, cancer cells
invade and damage the local surrounding tissue.
2. Spread to lymph channels and lymph glands (nodes)
Some
cancer cells may get into local lymph channels. (The body contains a
network of lymph channels which drains the fluid called lymph which
bathes and surrounds the body's cells.) The lymph channels drain lymph
into lymph nodes. There are many lymph nodes all over the body. A cancer
cell may be carried to a lymph node and there it may become trapped.
However, it may multiply and develop into a tumor. This is why lymph
nodes that are near to a tumor may enlarge and contain cancer cells.
3. Spread to other areas of the body
Some
cancer cells may get into a local small blood vessel (capillary). They
may then get carried in the bloodstream to other parts of the body. The
cells may then multiply to form secondary tumors (metastases) in one or
more parts of the body. These secondary tumors may then grow, invade and
damage nearby tissues, and spread again.
Cancer Staging
Staging is a way of
describing how much a cancer has grown and spread. A common way of
staging cancer is called the TNM classification:
- T stands for tumor - how far the primary tumor has grown locally.
- N stands for nodes - if the cancer has spread to the local lymph glands (nodes).
- M stands for metastases - if the cancer has spread to other parts of the body.
When a cancer is staged, a number is given for each of these three characteristics. For example, in stomach cancer:
- T-1
means the primary tumor is still in the stomach wall. T-3 means the
primary tumor has grown right through the stomach wall and T-4 means it
is invading nearby structures such as the pancreas.
- N-0 means
there is no spread to lymph nodes. N-1 means that some local lymph nodes
are affected. N-2 means more extensive spread to local lymph nodes.
- M-0
means there are no metastases. M-1 means that there are metastases to
some other area of the body such as the liver or brain.
So,
for a certain case of stomach cancer, a doctor may say something like
"the stage is T-3, N-1, M-0" which means "the cancer has spread through
the stomach wall, there is some spread to local lymph nodes, but no
metastases in other parts of the body".
There are other staging
classifications which are sometimes used for various cancers. For
example, a number system is used for some cancers. That is, a cancer may
simply be said to be stage 1, 2, 3 or 4 (or stage I, II, III, or IV).
Again, the stages reflect how large the primary tumor has become, and
whether the cancer has spread to lymph nodes or other areas of the body.
It can become complicated as each number may be subdivided into a, b,
c, etc. For example, you may have a cancer at stage 3b. A grade 4 stage
is often referred to as an advanced cancer.
Cancer Grading
Some cancers are also graded. A sample of the cancer (a biopsy) is
looked at under the microscope or tested in other ways. By looking at
certain features of the cells, the cancer can be graded as low,
intermediate or high.
- Low-grade means the cancer cells tend
to be slow-growing, look quite similar to normal cells (are well
differentiated), tend to be less aggressive, and are less likely to
spread quickly.
- Intermediate-grade is a middle grade.
- High-grade
means the cancer cells tend to be fast growing, look very abnormal (are
poorly differentiated), tend to be more aggressive, and are more likely
to spread quickly.
Some cancers have a slightly different
system of grading. For example, breast cancers are graded 1, 2 or 3
which is much the same as low-grade, intermediate-grade and high-grade.
Another example is prostate cancer which is graded by a Gleason score.
This is similar to other grading systems with a low Gleason score
meaning much the same as low-grade, and a high Gleason score meaning
much the same as high-grade.
For some cancers, a doctor will use
the information about the grade as well as the stage of the cancer when
advising about treatment options, and when giving an opinion about
outlook (prognosis).
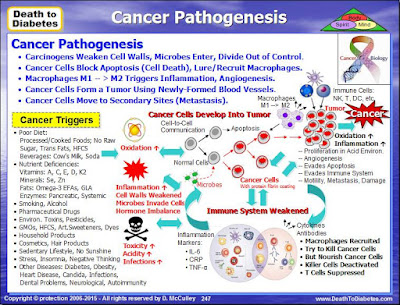
Cancer Pathogenesis
The
cancers with the highest growth rates had the highest fermentation
rates. The slower a cancer grew, the less it used fermentation to
produce energy. - See more at:
http://www.cancerfightingstrategies.com/oxygen-and-cancer.html#sthash.s35ok650.QfSwbilj.dpuf
The following
diagram is a high level depiction of how a general cancer develops in
the human body. Refer to the training program or science ebook for more
details.
Please Note! DNA damage is not the
cause
of cancer! Something caused the DNA to be damaged. Blaming the cause of
the cancer on DNA damage is like blaming smoke as the cause of a fire.
Instead it appears that there are several biological dysfunctions that damage or mutate DNA
and alter genetic expression, allowing cancer to proliferate. These biological dysfunctions include the following:
-- Chronic inflammation
-- Free radical damage (oxidative stress)
-- Hormonal imbalances
-- Toxicity overload
-- Chronic infections -- Nutritional deficiencies
Another concept about how cancer develops is the belief that the aforementioned biological dysfunctions trigger (pleomorphic) microbes to penetrate the cell
wall, which has been weakened by inflammation, oxidation, toxic foods and a toxic environment.
Once inside the cell, these microbes intercept the incoming glucose, and,
then, begin to multiply and secrete mycotoxins, creating an acidic
environment within the cell. In the meantime, the cell cannot function
because of the low ATP and acidic environment and the cell becomes a
cancer cell. Eventually, the toxic environment in combination with some
of the microbes invading the nucleus and causing damage to the cell's
nucleus, leads to the DNA and genes (in the nucleus) becoming damaged.
Of
course, how cancer develops is a lot more complex than this. We will
get into more details of cancer pathogenesis and pathophysiology in
future blog posts; and, also in the science book and training program.